Healthy Aging Physical Therapy Monthly Blog
Taking ‘OneStep’ Forward Towards Better Walking and Balance Outcomes
Healthy Aging Physical Therapy is excited to introduce OneStep in 2026 — an innovative smartphone-based tool that allows our clinicians to objectively measure gait, balance, and fall risk both in person and remotely. Learn why gait is considered the “sixth vital sign” and how OneStep helps us personalize care, track progress, and identify early signs of decline for older adults, people with Parkinson’s disease, orthopedic concerns, and balance or vestibular conditions.
Written By: Dr. Katie Wadland, PT, DPT, Owner: Healthy Aging Physical Therapy
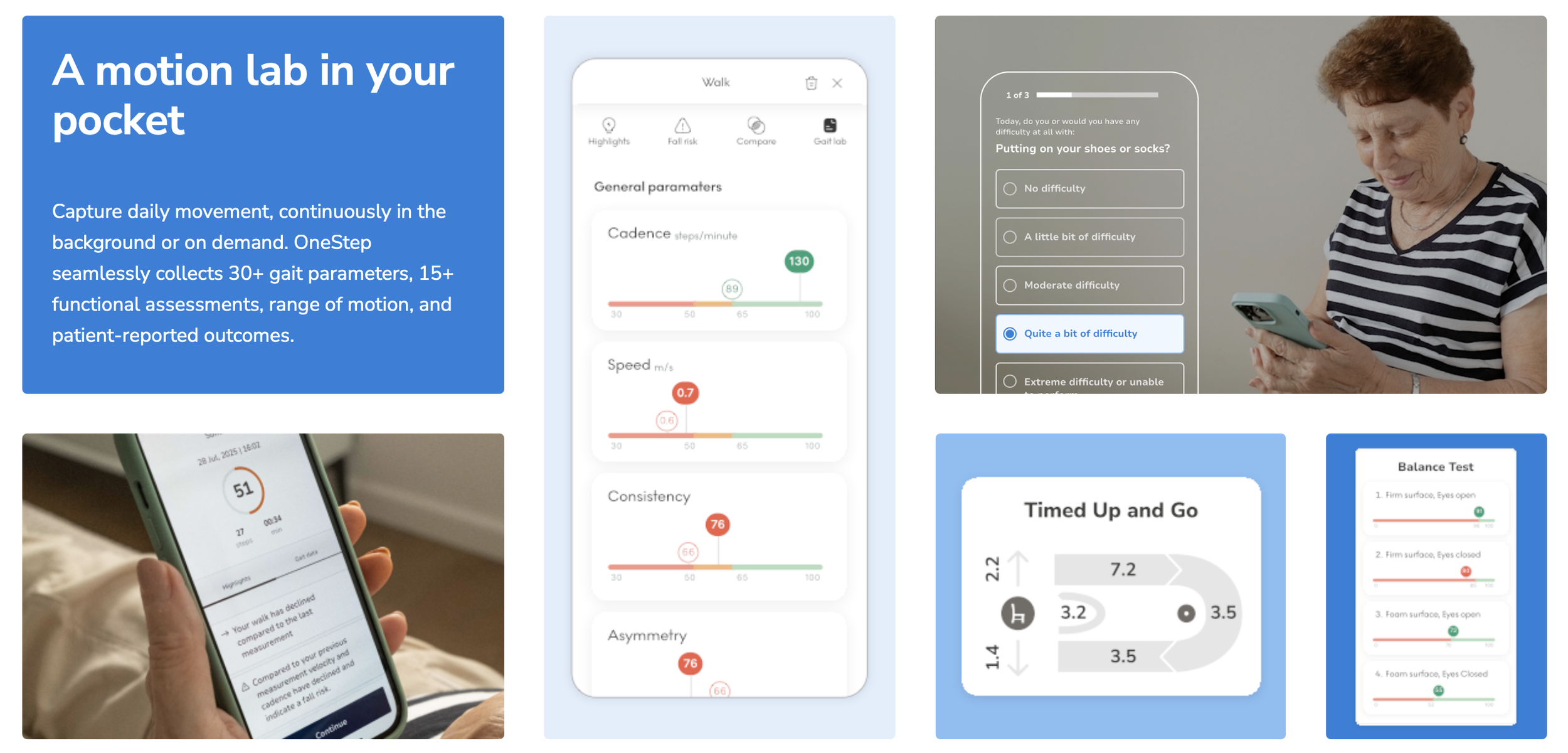
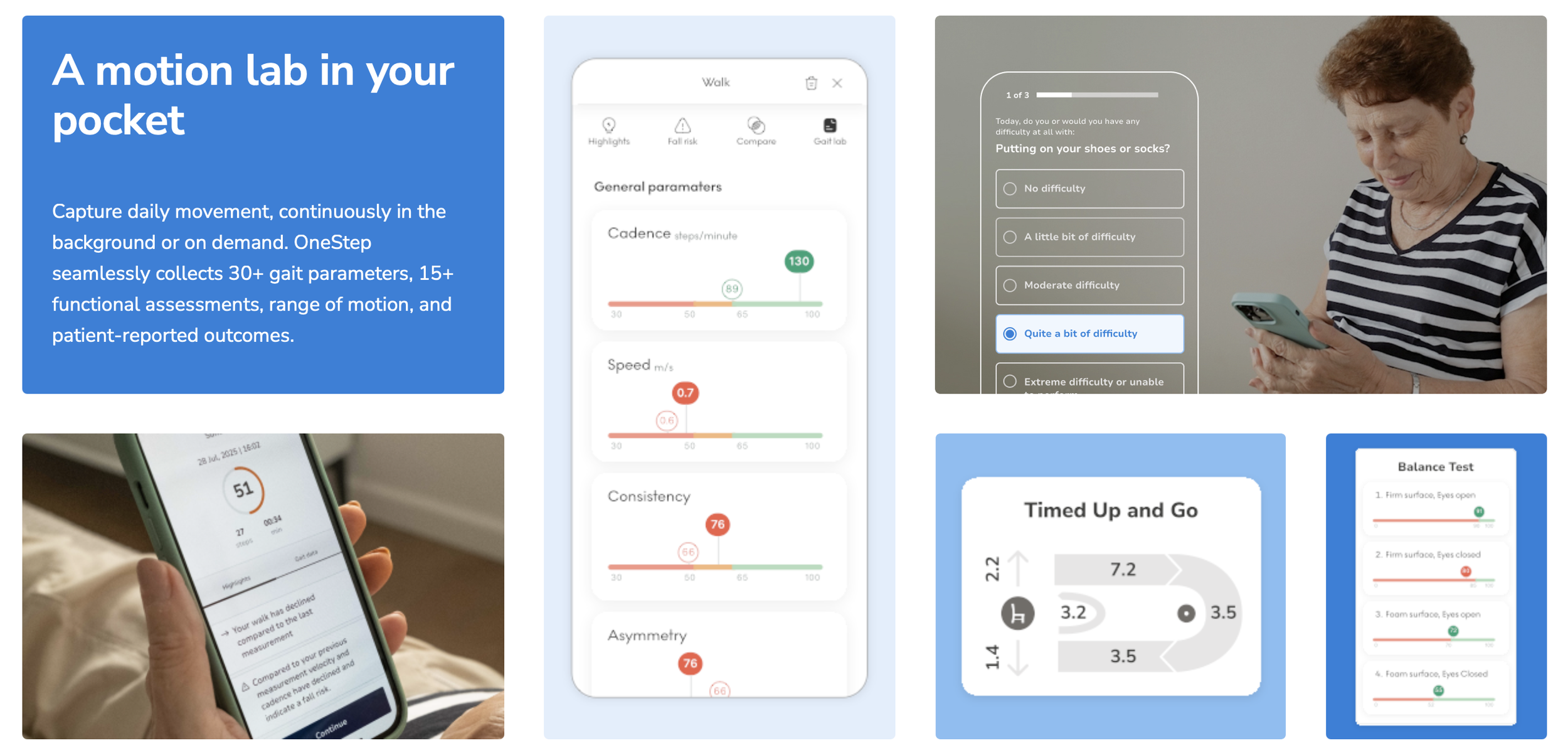
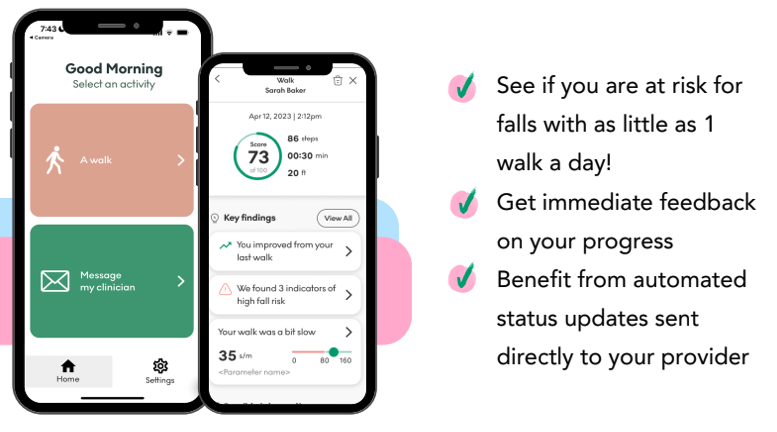
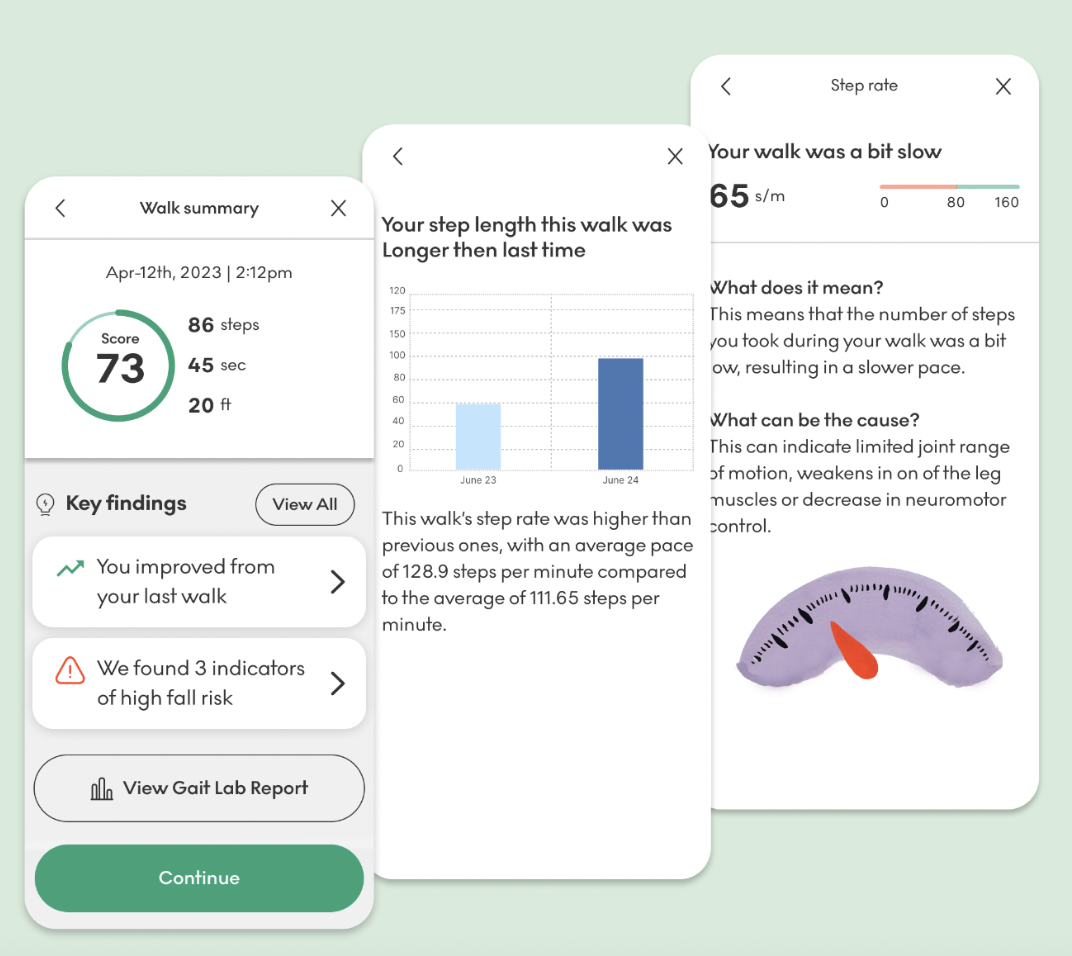
At Healthy Aging Physical Therapy, our mission is to deliver the most effective, evidence-based care available. That’s why we’re excited to introduce OneStep, a cutting-edge clinical gait analysis and remote monitoring platform we’ll begin offering to patients in February 2026. OneStep transforms a patient’s smartphone into a clinical-grade motion laboratory, allowing us to capture high-fidelity gait and mobility data both in clinic and in real-world environments using the device you already carry.
By simply putting a phone with our OneStep app in your pocket while you move around, we can:
Quantify walking speed, stride length, cadence, movement symmetry, variability, balance indicators, and other spatiotemporal gait metrics, all critical indicators of mobility and fall risk.
Detect fall risk and mobility decline earlier, enabling proactive adjustments to your care plan.
Monitor progress objectively and continuously throughout your plan of care - entirely remotely.
Improve patient engagement by showing concrete progress data rather than relying solely on subjective reports.
OneStep’s dashboard synthesizes movement into actionable clinical insights, helping your therapist tailor interventions based on quantitative evidence rather than estimation.
Evidence and Clinical Value
The scientific community increasingly recognizes gait, and particularly gait speed, as a key indicator of health. In fact, walking speed is referred to as the “sixth vital sign” because of its strong predictive value for functional decline, fall risk, future disability, hospitalization, and even longevity.
Beyond just “how fast” someone walks, gait characteristics reflect the integrated functioning of multiple physiological systems, including cardiovascular, neurological, and musculoskeletal health. Slower gait speed has been shown in multiple studies to correlate with increased risk of falls and adverse outcomes across older adult populations.
But Does it Work?
Peer-reviewed research has validated that smartphone-based gait analysis applications can provide reliable alternatives to traditional motion-laboratory measures and are feasible for evaluating gait dysfunction in clinical settings.
This supports our confidence that OneStep’s data is not just convenient, it is clinically meaningful and can augment traditional evaluation tools to give a fuller, real-world view of your mobility and fall risk.
Furthermore, OneStep’s own performance metrics (derived from aggregated real-world use) demonstrate its value:
The platform has analyzed tens of billions of steps and been used in mobility assessments for hundreds of thousands of patients, extracting 30+ gait and mobility parameters that clinicians rely on.
Organizational outcomes reported on OneStep’s platform include reductions in falls, improvements in patient engagement, and measurable time savings for clinicians, underscoring its operational as well as clinical impact.
Why This Matters to You
Traditional gait and balance assessments that we perform with you at home remain an essential part of your care. However, they are ultimately momentary snapshots of how you walk in that specific moment, often while your therapist is standing close by, observing, cueing, or providing supervision.
For many people, this setting does not fully reflect natural walking patterns. The presence of a clinician can unintentionally change how someone moves. Increased focus, heightened awareness, performance pressure, or a sense of being “watched” can lead to walking faster, more cautiously, or with more effort than usual. In some cases, people walk better than they typically do day to day; in others, they move more stiffly or guarded than normal.
As a result, what we see during a single assessment may not capture:
How you walk when you are relaxed and moving naturally
How fatigue, distraction, or multitasking affect your gait
How your walking changes throughout the day or across environments
Early signs of decline that emerge gradually rather than suddenly
By combining in-person clinical assessments with real-world gait monitoring, we gain a more complete and accurate picture of your mobility. This allows us to tailor your care not just to how you can walk when supervised, but to how you actually walk in daily life.
OneStep extends this model by providing:
Continuous monitoring across environments and times, capturing variations that might be missed in a single clinic visit.
Objective, quantifiable progress tracking instead of subjective impressions alone.
Early identification of decline or risk, allowing timely intervention before issues result in falls or functional loss.
This translates into more personalized care, more meaningful outcomes, and the ability to tailor interventions with precision.
Why Gait Matters for the Populations We Serve
While gait is a powerful health indicator across the lifespan, it is especially meaningful for the populations we work with every day. Subtle changes in walking patterns often appear before patients notice functional decline — and long before a fall, injury, or loss of independence occurs.
Older Adults
In older adults, gait speed, variability, and symmetry are strongly associated with:
Fall risk
Frailty progression
Loss of independence
Hospitalization and mortality risk
Even small reductions in gait speed (as little as 0.05–0.10 m/s) have been shown in research to represent clinically meaningful decline. Conversely, measurable improvements in gait speed correlate with improved survival and functional outcomes.
By tracking gait longitudinally, OneStep allows us to:
Identify early decline before it becomes a crisis
Distinguish “normal aging” from actionable impairment
Objectively measure improvement from strength, balance, and mobility interventions
Monitor mobility over time for patients on maintenance or wellness-based plans of care
For many older adults, gait truly reflects the intersection of strength, balance, endurance, cognition, and confidence.
Parkinson’s Disease and Other Neurologic Conditions
In Parkinson’s disease, gait is one of the most sensitive indicators of disease progression and functional impact. Changes in gait often include:
Reduced stride length
Shuffling or festination
Increased gait variability
Asymmetry
Freezing episodes
Reduced arm swing and trunk rotation
These changes can fluctuate day-to-day based on medication timing, fatigue, and environment — meaning they are often missed during brief clinic assessments.
With OneStep, we can:
Quantify changes in stride length, cadence, and variability over time
Monitor real-world walking, not just “best performance”
Identify subtle decline earlier and adjust interventions proactively
Better individualize cueing strategies, amplitude-based training, and balance work
Help monitor for changes in mobility related to medications, DBS and other therapies
This data supports more precise, responsive care, particularly for individuals living with Parkinson’s disease who benefit from long-term monitoring and early intervention.
Orthopedic Conditions
For patients with orthopedic concerns, including joint replacements, arthritis, spine conditions, or lower-extremity injuries, gait often compensates long before pain fully resolves.
Common gait-related issues include:
Asymmetrical loading
Reduced stance time on the involved limb
Altered cadence or step length
Persistent compensations that increase stress on other joints
OneStep allows us to:
Objectively assess symmetry and loading patterns
Track recovery beyond pain reduction alone
Ensure gait normalization, not just task completion
Identify lingering deficits that may increase reinjury risk
This helps ensure that “feeling better” also means moving better, reducing long-term wear and injury risk.
Balance and Vestibular Conditions
For patients with vestibular disorders or balance impairments, gait often reveals deficits that static balance tests do not.
Changes may include:
Increased gait variability
Slower walking speed
Widened base of support
Hesitancy or avoidance in real-world environments
Because balance confidence and sensory integration vary by environment, gait measured outside the clinic provides critical insight.
With OneStep, we can:
Assess dynamic balance during everyday walking
Monitor response to vestibular rehabilitation over time
Identify sway and movement during static balance assessments
Better tailor progression of dynamic balance and dual-task training
This allows us to move beyond symptom resolution toward true functional confidence and safety.
Want to Take ‘OneStep’ Closer to Better Walking and Balance With Us?
Beginning in February 2026, OneStep will be integrated into care at Healthy Aging Physical Therapy as part of our comprehensive assessment and treatment planning process.
During your evaluation or reassessment, your clinician may use OneStep to help measure and better understand your walking and balance. In some cases, we may ask you to download the OneStep app to your phone and use it as a way for us to track gait and mobility data over time during your plan of care - both in person and, when appropriate, remotely.
There is no additional cost to you for using OneStep during skilled physical therapy.
You can expect your clinician to:
Explain how OneStep works and how it uses your phone to measure walking
Review which gait and mobility metrics are relevant to your goals
Use this information to more precisely tailor your treatment plan and monitor progress or change over time
Interested in Gait Insights, but not a Current Patient?
If you’re interested in understanding your gait, balance, or fall risk, but are not in need of skilled physical therapy services, you may request a Wellness Evaluation through our Wellness365 Program. This allows you to experience OneStep, receive objective gait data, and gain professional insight into your movement patterns outside of an insurance-based plan of care. We will also be rolling a third tier in our Wellness365 program to allow for long term engagement with your therapist and ongoing monitoring of your gait, mobility and exercise program so stay tuned for more details!
Gait is more than movement - it is a vital signal of health. OneStep gives us a powerful, data-driven way to listen. If you have questions or would like to learn more, we’re happy to talk with you.
Looking Back, Looking Forward and Steve’s Story
How outpatient-at-home therapy and wellness services support older adults through care transitions - one patient’s journey from therapy to long-term strength.
By: Dr. Katie Wadland, PT, DPT, Board-Certified Geriatric Clinical Specialist
Owner: Healthy Aging Physical Therapy
Looking Back
Healthy Aging Physical Therapy started in 2020, at a time when healthcare, and daily life, felt especially fragile.
Older adults were losing access to care. Families were stretched thin. Healthcare systems were overwhelmed. I didn’t start this practice with the goal of building something large or disruptive. I started it because I knew I could help a small number of people in a way that felt safe, practical, and personal, by seeing them in their homes and reducing barriers to quality care.
While this mindset hasn’t changed much over the years, what has changed is the scope. In 2020, we helped 24 patients. In 2021, that number grew to 119. In 2022, 312. By 2023, we were helping 436 people, and in 2024 that grew to 528. This year, in 2025, we’ve already helped 565 people through individual therapy alone.
Those numbers don’t include the patients we’ve continued working with year over year, or the group classes we run each month. On average, we now teach about 50 group classes a month, reaching roughly 240 people each week—more than 800 individuals over the course of a year.
I share these numbers not as a growth story, but as a reminder of how influence tends to build quietly. Most of this didn’t come from doing more things. It came from doing things differently—letting outcomes, relationships, and word-of-mouth carry more weight than advertising or polished messaging.
What I want to share is how those differences have evolved into a consistent way of caring for patients, our own, unique “Healthy Aging way,” and what that looks like through one patient’s experience.
Meet Steve
Steve’s story is a good example of how this plays out in real life.
We began working with Steve in May of 2025. About a year earlier, he had undergone a total knee replacement and experienced a series of complications that led to multiple hospitalizations. Before all of this, Steve lived independently, walked with a walker, and managed his own daily needs.
By the time we met Steve, his situation had changed significantly. He had moved into an assisted living facility, was using a wheelchair for all mobility, and required maximum assistance for transfers. Home health services had ended, and he had been advised that he would need to transition to outpatient therapy.
This is a familiar, and often challenging, moment for many patients. Home health and VNA services play a critical role during periods of medical instability and true homebound status, helping people recover safely and stabilize after illness, injury, or hospitalization. As patients improve and no longer meet homebound criteria, those services appropriately come to an end.
At that point, many individuals have regained some function but haven’t yet returned to their prior level of independence. They’re often encouraged to transition to clinic-based outpatient therapy or continue on their own with a home exercise program. Some are able to make that transition. Others find outpatient-at-home providers like us. And many, simply, fall through the cracks.
In Steve’s case, clinic-based outpatient therapy wasn’t a realistic option. Getting in and out of the car safely and consistently just wasn’t feasible. He was no longer driving and didn’t have regular access to transportation, which is what led to his referral to us for outpatient-at-home care.
Steve began working with one of our physical therapists and stayed in skilled therapy for as long as his insurance allowed. Over time, he made steady, meaningful progress. Strength improved. Transfers became easier. When Steve was discharged from skilled physical therapy in early November, he was no longer using a wheelchair. He was walking with a rollator and, at times, a cane. He had returned to working part-time. His level of independence looked very different than it had just months earlier. He had met his therapy goals - and demonstrated capacity beyond them.
By insurance standards, this was an appropriate place to stop, but as we find time and time again, function doesn’t always fit neatly into coverage timelines.
Next Steps (Literally!)
One thing we see often is that patients lose momentum after therapy ends—not because they’ve reached their limit, but because the structure and support that helped them improve suddenly fall away.
Steve and his physical therapist both felt there was more room to improve. While additional therapy visits weren’t covered at that point, Steve transitioned into our Wellness365 program to continue his work with our personal trainers. This shift allowed him to keep moving forward without the time limits or coverage restrictions that often shape insurance-based care.
The wellness setting also opens the door to goals that typically fall outside the scope of covered therapy - things like returning to hobbies, building higher-level strength and endurance, and focusing on overall health rather than just functional mobility and task completion. Steve’s training program evolved into a whole-body approach, combining strength, balance, and cardiovascular work. The focus wasn’t just on regaining function, but on building resilience and supporting his long-term health.
The result? Last week, one of our trainers shared a video of Steve climbing stairs, something simple to most of us, but incredibly meaningful for someone working toward independence again. It brought a smile to all of our faces that day.
While many patients experience decline after therapy ends, Steve has continued to gain strength and confidence. Not because he followed a perfect path, but because he stayed engaged and supported through transitions, with a team that could adapt his care as his goals, and his capacity, continued to grow.
Looking Forward
Steve’s story is just one example. Every patient’s path looks different. Some need short-term support, while others benefit from longer stretches of therapy, wellness, or a combination of both. Goals vary, timelines vary, and the right approach isn’t always the same from one person to the next.
What I’m most proud of this year is having built a practice that’s flexible enough to meet patients where they are—to adjust care as needs change, to support transitions rather than disrupt them, and to offer different options based on what works best for each individual.
That adaptability—and the ability to walk alongside patients through different phases of their journey—is what makes this work meaningful for our team, and what continues to guide how we care for the people we serve as the years go on.
Home for the Holidays: 10 Tips, Tricks, and Helpful Products to Improve Safety at Home - and When You’re Away from Home
Make this holiday season safer and more joyful for the older adults you love. In this post, Dr. Katie Wadland, PT, DPT, Board-Certified Geriatric Clinical Specialist and owner of Healthy Aging Physical Therapy, shares 10 practical tips, tricks, and affordable products to support aging in place—at home or while traveling. Learn how to manage energy, prevent falls, simplify travel, and choose smart gifts that promote safety, comfort, and independence.
By Dr. Katie Wadland, PT, DPT, Board-Certified Geriatric Clinical Specialist
Owner: Healthy Aging Physical Therapy
The holiday season brings joy, family, and togetherness — but also new challenges for older adults. Between traveling, hosting, and adapting to new environments, it’s easy to underestimate just how much energy it all takes. Whether you’re hopping on a plane or staying home in your coziest slippers, a little planning and the right tools can go a long way toward keeping the season safe and comfortable.
Here are ten of my favorite practical, therapist-approved strategies and helpful products to make your holidays easier — without sacrificing the fun.
1. Manage Energy Like It’s Money
One of the biggest challenges of the holidays is fatigue — not just physical, but mental. The social effort of being “on,” chatting with relatives, and maybe even trying to mask any impairments can be draining.
💡 Tip: Think of each day as a dollar — you have $1 to spend. How much will church cost? Dinner with family? A trip to the store for pie ingredients? Spend wisely.
If dinner with your daughter is the highlight, maybe let go of the baking marathon and supervise while the grandkids take over the kitchen.
🎁 Helpful Product: Super Ear Personal Sound Amplifier. Hearing clearly during conversation saves tremendous mental energy.
2. Prepare for Low Surfaces
That comfy couch at your daughter’s house? Not so comfy when you’re stuck in it. While you may confidently get on and off the chairs in your own home, visiting friends, family and restaurants may leave you feeling like Goldilocks trying out difference surfaces to find the ‘just right’ seat for you. Avoid getting stuck with the tips below:
💡 Tip: Start “training” now. Practice sit-to-stands from different surfaces, even try sitting on a pillow to simulate a lower seat.
🎁 Helpful Product: Carex Up Easy Seat Assist — portable, hydraulic seat lift that helps you rise with less strain.
3. Conquer Community Stairs
Even if your home has no stairs, public places or loved one’s homes might. Don’t let a ‘3 STE’ (three stair entry in PT short hand!) stop you from enjoying the festivities.
💡 Tip: Practice toe taps and step-ups at home to build balance and confidence.
🎁 Helpful Product: Try a Stair Cane, which is a lightweight and portable “travel railing” for those steps without rails anywhere or the Stair Assist which lets you create a '“half step” to bridge the gap between the floor and a high step up anywhere you need one.
4. Sleep Smart in New Spaces
Guest beds are often softer, lower, or lack support for getting up. Further, the trip to the bathroom is unfamiliar, and likely dark and dangerous. Solution? BYO-Nightlight and a couple of helpful hints for chair placement:
💡 Tip: Place a sturdy chair or walker next to the bed, and use portable nightlights to light your path to the bathroom.
🎁 Helpful Product: Battery-Powered Motion Nightlights — compact, battery-powered and great for travel.
5. Fly Easier
Air travel can be exhausting long before you board. Fortunately, TSA has excellent support services available not only to reduce strain, but to speed you through long lines and reduce energy cost of travel.
💡 Tip: Call ahead to schedule TSA Cares Assistance for any air travel you have coming up — they’ll escort you by wheelchair through security and to your gate, often bypassing long lines.
🎁 Helpful Product: Drive Medical Nitro Dual Function Rollator/Transport Chair — walk when you can, ride when you need to, this dual-function walker/transport chair is one of my favorites to recommend to my patients.
6. Drive Safely AND Comfortably
While driving cross country may have been doable in your youth, as we age, even short road trips can become more challenging and may require advanced planning.
💡 Tip: Plan for frequent stops, avoid driving tired or at night, and consider public transit or rideshares for longer trips.
🎁 Helpful Product: A portable Car Cane + Car Handle and a Lumbar Support pillow can make getting in and out a breeze, and long drives more comfortable.
7. Stay Connected from Home
If you’re celebrating quietly at home, you can still fill your space with connection and joy.
Smart speakers like the Echo Dot can:
Play your favorite holiday music (“Alexa, play Christmas music!”)
Set medication reminders
Control lights or thermostats
Call for help in an emergency
Get even fancier with an Alexa Show which has all the fun features of a Dot with the addition of a 15” screen so you can see your reminders, follow along with recipes, watch the local news and even see your calendar for the day.
8. Give the Gift of Comfort
Nothing says “I love you - and want you to be safe” like warm, slip-proof slippers and house shoes. Fan favorites in my house AND with my patients include the classic LL Bean Moccasin and the Hey Dude Shoes — both easy to slip on, stable, and cozy.
9. Give the Gift of Health
Aging well takes time, effort and often, support. The good news is that there are great devices and services available to help your loved one stay healthy and active at home. Consider purchasing a portable elliptical like the Cubii or setting them up with a ten pack of training sessions with us through our Wellness365 program. We can bring personal training right to your home, with specialists who understand the needs of older adults.
10. Give the Gift of Safety
Technology is amazing and wearable devices can bring convince, accessibility and peace of mind. Devices like the Apple Watch can now detect falls and call emergency services — a simple, life-saving feature for any older adult.
Final Thought
The holidays aren’t about doing everything — they’re about doing what matters most. Whether that means a little extra planning for your trip to the kids or asking for help at the airport, small choices can keep you safe, confident, and able to enjoy what really counts: time with the people you love.
From all of us at Healthy Aging Physical Therapy, we wish you a safe, warm, and joyful holiday season.
Cutting Through the Chaos: Creating Effective Frameworks for Complex Patients
Many older adults don’t fit neatly into a single diagnosis—and neither does their care. In Cutting Through the Chaos: Creating Effective Frameworks for Working with Complex Patients, Dr. Katie Wadland, PT, DPT, Board-Certified Geriatric Clinical Specialist, shares how Healthy Aging Physical Therapy helps clinicians and families navigate the challenges of treating medically complex patients. Learn how to identify priorities, layer support, and build collaborative care plans that promote safety, independence, and resilience for older adults with multiple conditions.
Written by: Dr. Katie Wadland, PT, DPT, Board-Certified Geriatric Clinical Specialist Owner: Healthy Aging Physical Therapy
If you’ve ever worked with, or been, a patient who seems to have more going on that meets the eye, you know how challenging it can be. Fortunately, these are also often the most rewarding patients - and, most importantly, the ones who need us most.
At Healthy Aging Physical Therapy, our team specializes in exactly that: caring for complex patients—people with multiple diagnoses, long medical histories, and functional challenges who often feel like no one knows where to start. They’re the ones who have seen five other therapists, have a dozen specialists, and still feel stuck.
Why Our Patients Are So Complex
When you’re in physical or occupational therapy school, you learn about impairments in isolation.
A hip fracture? You study how to rebuild strength and balance.
A cardiac patient? You learn to monitor vitals and improve endurance.
A neurological condition? You focus on motor control, coordination, and safety.
But real-world patients with geriatric, neurologic, and complex medical needs don’t fit in tidy boxes. The people we serve are living with multiple comorbidities, often taking many medications, and facing social and emotional challenges that go far beyond their diagnosis list.
For example, many of our patients with Parkinson’s disease also experience osteoarthritis, chronic pain, memory loss, anxiety, and depression - and often have a partner who is also aging and managing their own medical issues to boot. Similarly, a patient referred for “hip fracture” is rarely just an orthopedic case. The fracture may have resulted from a fall, which stemmed from a combination of weakness, balance impairments, cardiac symptoms, and home safety challenges. Many live alone, with limited support and a history of sedentary behavior.
It’s no wonder that walking into these homes for an evaluation can feel overwhelming, even for seasoned clinicians.
Many of these individuals have already been discharged from other settings because progress stalled, the situation was too complicated, or insurance coverage ran out. Over time, we’ve become the go-to practice for these patients—the ones other providers refer when they aren’t sure what else to do. In many cases, we become the last stop—the “hail Mary” for patients who are exhausted from circling through the healthcare system.
So, how do we help?
Our Framework for Treating Complex Patients
Through experience and teamwork, we’ve developed a simple, realistic framework that helps our clinicians navigate these challenging situations - one that keeps both patient and therapist grounded, hopeful, and effective.
Whether you’re a therapist reading this, a patient with a complex background, or a caregiver trying to support a loved one, I hope these strategies help you cut through the chaos and find a starting point that leads to progress.
1. Focus on What Matters Most and Not Everything at Once
When faced with a dozen problems, it’s natural to want to fix them all. But that’s a recipe for overwhelm, and, inevitably, an ineffective therapeutic approach.
Instead, we teach our therapists to start by asking:
“What are the top one or two things we can help with right now that will most improve this person’s quality of life, safety, and independence?”
Sometimes that means addressing strength, balance, or mobility. Other times, it’s about helping the patient move again after weeks (or months) of fear and inactivity. Sedentary behavior, whether from pain, fear, or fatigue, triggers a cascade of physical and emotional decline and often, interrupting this cycle can be an important first step. Even small steps toward safe, confident movement can change everything. Sometimes, a compensatory approach is the right starting point: helping a patient obtain the proper wheelchair, walker, or other durable medical equipment to restore access to their home and community.
Time after time, we’ve learned that small wins matter. They build trust, confidence, and momentum - all critical ingredients for rapport and long-term success.
2. Layer in Support
We remind our team (and ourselves) that we can’t fix everything - and that’s okay. Somethings aren’t ‘fixable’ and other things are outside of our scope and capabilities.
Our role is to make a meaningful difference where we can, while also building a web of support around the patient to provide support for ‘the other things’. That often means:
Connecting patients with mental health providers when mood disorders or anxiety is a barrier
Coordinating with care team physicians and pharmacists to address medication-related issues
Referring our patients to trusted home health aides, elder services, or aging life-care specialists
Providing resources for community programs, support groups, and case managers
It’s not about doing it all ourselves - it’s about building the right team around each patient, one layer at a time.
3. Collaboration Is Key
When you work with a Healthy Aging therapist, you may only see one person walk through your door—but behind that therapist is an entire network of expertise.
Our team includes specialists in neurology, orthopedics, geriatrics, vestibular therapy, and cardiopulmonary rehab. We collaborate behind the scenes through discussion boards, case consults, and joint visits - bringing fresh ideas, new eyes and diverse perspectives to every complex case. Sometimes that collaboration means I’ll step in for a Complex Case Visit, working alongside the treating therapist to strategize solutions. Other times, the team shares insights online, helping each other troubleshoot mobility challenges, medication effects, or behavioral barriers.
That culture of teamwork is one of our greatest strengths—and one of the biggest reasons I feel our patients make progress where others have stalled.
4. Think Long-Term
Complex patients rarely fit neatly into a six-week plan of care. Their needs evolve, new issues arise, and maintaining stability often becomes the goal as much as improvement.
That’s why we emphasize continuity - treating each patient as someone we’ll likely know for years. When a patient is ready to discharge, we make sure:
A comprehensive post-discharge home program is in place
The patient has been connected with the appropriate community and medical supports
We have established a clear plan for future follow-up
For many, we transition them into a Maintenance Plan of Care under Medicare Part B, or into our Wellness program, Wellness365, where they continue to receive guided exercise and ongoing support to prevent decline.
Because our ultimate goal isn’t just short term rehab - it’s recovery and resilience.
What This Means for Patients and Families
If you’re a patient, caregiver, or family member feeling frustrated that “no one knows how to help,” please know: you’re not alone, and your situation isn’t hopeless.
Working with complex conditions takes time, teamwork, and the right perspective. The most important first step is finding professionals who know how to cut through the chaos - and, most importantly, who see you as a person first, not just a list of diagnoses, which is the heart of what we do at Healthy Aging Physical Therapy.
Why More Seniors Are Choosing At-Home Physical & Occupational Therapy
Learn the top 5 reasons older adults are referred for outpatient physical and occupational therapy at home — including fall risk, Parkinson’s care, post-hospital recovery, and more. Discover how at-home PT and OT from Healthy Aging Physical Therapy can help you stay safe, strong, and independent.
By: Dr. Katie Wadland, PT, DPT, Board-Certified Geriatric Clinical Specialist and
Owner of Healthy Aging Physical Therapy
At Healthy Aging Physical Therapy, we specialize in bringing expert care to your doorstep. Outpatient at-home therapy means you get the same high-quality physical or occupational therapy you'd receive in a clinic — but in the comfort, safety, and convenience of your home.
So, why do patients (and their doctors!) turn to us?
Here are the Top 5 Reasons we get referrals for outpatient at-home PT and OT:
1) Fall Risk & Balance Issues
Let’s start with the biggest one — fall prevention.
Falls are the leading cause of injury and hospitalization in older adults, and 60% of them happen at home.
By treating balance issues where they happen most — in the actual environment you live in — we can make a major impact on your safety. Our therapists assess your home for hazards, recommend simple modifications (like grab bars or lighting changes), and provide targeted balance training to reduce your fall risk and keep you confident and independent.
This is our #1 reason for referral — and for good reason. Learn more about our Balance and Falls Program Here
2) Difficulty Leaving the House
Getting to the clinic isn’t always easy. Many of our patients no longer drive, rely on family or caregivers for rides, or find the process of getting ready, getting out, and getting home exhausting.
With outpatient-at-home therapy, we eliminate the transportation barrier and bring care straight to you.
That means you get to use your energy for your session — not the drive — and caregivers get a break from extra errands and logistics. Plus, we often find better focus, higher participation, and more consistent follow-through when therapy is done at home.
3) Parkinson’s Disease
We specialize in helping individuals with Parkinson’s Disease live fuller, more active lives.
Our therapists and trainers are certified in PWR! Moves, an evidence-based therapy program designed specifically for people with Parkinson’s — and our PD program goes far beyond just therapy.
We offer:
Individualized PT & OT
Group fitness classes tailored for Parkinson’s
Personal training with PD-certified instructors
Complex case management
Home safety evaluations and cognitive support strategies
From diagnosis to long-term maintenance, we’re with you every step of the way.
📘 Learn more about our Parkinson’s Program Here
4) Recent Hospital Stay
Even a short hospital stay can cause serious weakness and deconditioning in older adults. Research shows that just 48 hours in a hospital can lead to muscle loss, reduced balance, and increased fall risk.
Whether you were hospitalized for an illness, injury, or surgery, therapy is often essential to helping you get back on your feet — and back to your prior level of function.
We meet you at home as soon as you're ready, and help build a plan to regain your strength, restore your confidence, and safely resume your daily routines.
5) Back & Joint Pain
As we age, it’s common to experience arthritis, spinal degeneration, and general wear-and-tear that leads to aches, pains, and stiffness.
But here’s the difference: While orthopedic clinics often treat just the pain site, our geriatric specialists take a whole-body, whole-person approach — looking at your posture, strength, mobility, balance, and lifestyle. We help you reduce pain and improve how you move, so you can stay active and avoid future injuries.
Why At-Home Therapy Works
Outpatient-at-home therapy is not home health care — it’s the same outpatient services you’d receive in a clinic, but delivered at home. We’re fully licensed, accept Medicare Part B and most managed Medicare plans, and provide:
1:1 focused sessions
Expert therapists and assistants
Continuity of care with the same provider
A personalized, goal-driven approach
📘 Learn more about Outpatient at Home Physical Therapy or Occupational Therapy here.
Want to Learn More?
📞 Give us a call or talk to your provider about a referral. You can register online for a new evaluation by following the link below: