Healthy Aging Physical Therapy Monthly Blog
Should I use a Cane or a Walker?
FAQ: Should I use a Cane or a Walker?
The answer is...it depends! (This is every physical therapist's favorite answer, by the way...)
As a Geriatric Physical Therapist, I spend oodles of time talking about assistive devices. Whether it’s working to wean off of one, or educating my patient on the importance of using one, my day-to-day includes much talk of canes, walkers, wheelchairs and the like. But like most things in PT-world, the who-gets-what assistive device conversation is never black and white, but here are a few things I think about when deciding which assistive device to recommend.
The answer is...it depends! (Shocking, right?)
As a Geriatric Physical Therapist, I spend oodles of time talking about assistive devices. Whether it’s working to wean off of one, or trying to convince my patient to use one, my day-to-day includes much talk of canes, walkers, wheelchairs and the like. But like most things in PT-world, the who-gets-what assistive device conversation is never black and white. That said, here are a few things I think about when deciding which assistive device to recommend.
Should I walk with a Cane?
These are your run of the mill straight stick supports like the guy is using above. They can have flat tops or curved; sometimes people buy fancy tripods to help them stand up or ice picks to add to the bottom to use in the winter. They come in all shapes and sizes, but have one thing in common - they will not stop you from falling if your legs give out. So, my first factor in determining whether to recommend a cane is strength. Basically, if you’re going to use a cane, you need to have enough strength to walk at least the distance you’ll be using it to walk (household or community) a couple of times in a row securely. The second factor I consider is balance. While a cane is great for folks who have minor balance impairments, you really need to have adequate reactive responses (the ability to catch your balance if you do start to fall) to make walking with a cane safe. The last thing I generally think about is coordination. Some people, (no judgement here..) are just not ‘cane-people’. Instead of helping, it becomes a hindrance. If the idea of using a cane seems overwhelming, requires a lot of focus or becomes another item to trip over, it probably isn’t the device for you. In fact, these are the folks I actually tend to focus towards without a device.
Does using a cane help with pain?
I tend to use canes for my folks that have pain. A cane is a GREAT way to reduce load on a painful joint - whether temporarily or ongoing as part of a pain management plan. Another pro for canes - it helps people walk with a more natural gait pattern (good for brain = good for gait). But there’s a catch - if you use a cane on the wrong side (the side CLOSEST to the painful side), you actually increase the load and as a result, the pain. So, if you’ve got a painful right knee, the cane needs to go on the left so when you step onto that side, the cane is there to support it. I won’t go into much detail about the other cane options (large-based or small-based quad canes), because quite frankly, I don’t like them. It is hard for people to remember which way to use them (flat side goes toward you FYI), they get under-foot quite easily, and generally slow people down. Yes, they have their purpose for a small group of folks (like people with hemiplegia after a stroke) but for our general purposes today, I’ll leave them in them out of the discussion.
Should I walk with a Walker?
Walkers, like people, come in all shapes and sizes, and vary in quality. The old silver one with the wheels in the front and legs in the back is called a Rolling Walker. Four legs without wheels is a Standard Walker. (To save some time and energy, the only time a standard walker is going to the the ‘right answer’ is if you aren’t allowed to put full weight on your leg, or if you are missing a leg. Case Closed.) Despite the fact that we’ve developed crazy things like the INTERNET in the last hundred years, the design of these two basics actually haven’t changed much, if at all. These are the kinds of walkers you’ll come home from the hospital with if you’ve had a joint replacement or experience a fall and fracture. While the rolling walker has it’s time and place, and is certainly the safest option *in-home* for many people, it is not my favorite device. Using a rolling walker a) limits your speed (bad for brain = bad for gait), b) limits your trunk rotation and arm swing (again bad for brain = bad for gait) and c) frequently leads, in my opinion, to increased isolation because people often either don’t want to be seen by their neighbors and friends with a walker, or just find the darn thing cumbersome. I put *asterisks* around *in-home,* because my biggest walker pet-peeve is they are HORRIBLE for walking on most suburban streets and sidewalks. While they may work well l if you live in a brand new town with perfectly manicured roadways, where I live, between tree-roots and frost heaves, most areas I gait-train with patients are basically a head-over-heels situation waiting to happen. Watching a patient try to navigate uneven terrain with a rolling walker is not my favorite experience. Walkers don’t work on grass, they don’t work on sand, and in reality, they don’t work too well on sidewalks.
What is the best Walker to buy?
Enter the Rollator. Rollators get a bad rap because they move fast and because the brakes get loose, but I actually prefer to wean a patient onto a rollator when I can. Rollators, with their four wheels + hand brakes and a built-in chair, give a person an option for life outside of their home (in my humble opinion). Using a rollator, for most people, is more intuitive than a walker; it actually turns in a circle and makes turning corners way easier, it is smoother over uneven sidewalks, can actually go over grass - and my favorite, allows you the freedom to walk further because you have an option to sit and take a break when you need to! Rollators make great choice for someone who may be limited by balance, endurance, cardiopulmonary impairments or back pain, but who still would like to be able get out and about in their communities. Quick note about rollator quality: while the general ‘got it for free from a neighbor’ rollator may not be the best, when a patient can afford it, I usually recommend a sturdier model called the Nitro. It is heavier, but stronger, more secure and is like the SUV of rollators. (Nitro Walker)
Still wondering if a Cane or a Walker or Nothing at All is the right thing for you? Ask a PT:)
We are movement experts; our job is to help you find the safest way to navigate your environment while at the same time, giving you the maximum independence. For some, this may mean weaning off an assistive device; for others, it may means encouraging you to use one. The Cane Vs. Walker Showdown is rarely black and white. What may work in your home may not be what is best for use in the community. You may be able to use a Cane or Nothing at All during the day, but a Walker may be best at night. See, like I said…It Depends:)
About the author:
Dr. Katie Wadland, PT, DPT is the Owner and Primary Physical Therapist at Healthy Aging Physical Therapy. Healthy Aging Physical Therapy offers in-home Physical Therapy for older adults living in Melrose, Medford, Arlington, Stoneham, Winchester, Reading, Woburn, Wakefield and Lynnfield, Massachusetts. She is licensed to practice Physical Therapy in the State of Massachusetts (License #18193). She has over fourteen years of experience working with older adults with musculoskeletal and neurological impairments and advanced training in the care of people with Parkinson’s Disease, Spinal Cord Injury and Stroke.
What is Health Literacy - and Why Does it Matter?
During a library talk last week, I spoke on the topic of Health Literacy. The day I was scheduled to present, I found myself dealing with a real-life example with a patient of why having a good grasp on health literacy is so critical to healthy aging. During our visit, I realized my patient had been taking double the dose of her prescribed medication - not out of any error on her part, but because she had two prescriptions on file for the same medication, one for the generic version, and one for the brand name - and she was unaware they were the same drug. How does this happen? How does it get by so many layers of well-meaning and conscientious health care professionals and hospital settings? Unfortunately, this stuff happens, and happens all too often, because there are a lot of ‘cooks in the kitchen’ and because all of us ‘cooks’ are human and we make mistakes. But this, this is why it is so imperative for you as the consumer, as the patient, to have an adequate level of health literacy - so you can be your own advocate, so you can be on the lookout for these human errors and so you can play an active, instead of passive, role in your own health maintenance.
During a library talk last week, I spoke on the topic of Health Literacy. As life would have it, the day I was scheduled to present, I found myself dealing with a real-life example with a patient of why having a good grasp on health literacy is so critical to healthy aging. During our visit, I realized my patient had been taking double the dose of her prescribed medication - not out of any error on her part, but because she had two prescriptions on file for the same medication, one for the generic version, and one for the brand name - and she was unaware they were the same drug. How does this happen? How did this get by so many layers of well-meaning and conscientious health care professionals and hospital settings? Unfortunately, this stuff happens, and happens all too often, because there are a lot of ‘cooks in the kitchen’ and because all of us ‘cooks’ are human and we make mistakes. But this, this is why it is so imperative for you as the consumer, as the patient, to have an adequate level of health literacy - so you can be your own advocate, so you can be on the lookout for medical errors and so you can play an active, instead of passive, role in your own health maintenance.
What is Health Literacy?
“Health literacy is the ability to obtain, read, understand and use healthcare information in order to make appropriate health decisions and follow instructions for treatment.” (Wikipedia).
Sounds simple enough, right? It may be simple enough if you have one or maybe two medical diagnoses, or take a pill or two in the morning. But what happens when the list starts to add up? When you’re taking pills in the morning, a few after lunch and one before bed? When the instructions come from more than just your primary care physician, but also from your cardiologist or neurologist? If you’ve ever been discharged from the hospital, you’ve had the experience of being issued a stack of papers to sign with discharge recommendations, red flags to be aware of, with a current medication list (which may have new pills or have old pills crossed off) and visits you’ll need to attend in the future. This experience alone is overwhelming. Add in confusion, fatigue, pain or anxiety related to your hospital stay and you now have a recipe for disaster. It is REALLY HARD to keep track of it all, and even harder to keep up with the changes that are often part of getting older and dealing with chronic diseases, new diagnoses, illnesses and injuries.
How do you know if you are adequately health literate?
You may be responsible for not only your health information management, but also for a spouse or aging parent.
At the minimum, to be health-literate, you should have a solid grasp on the following:
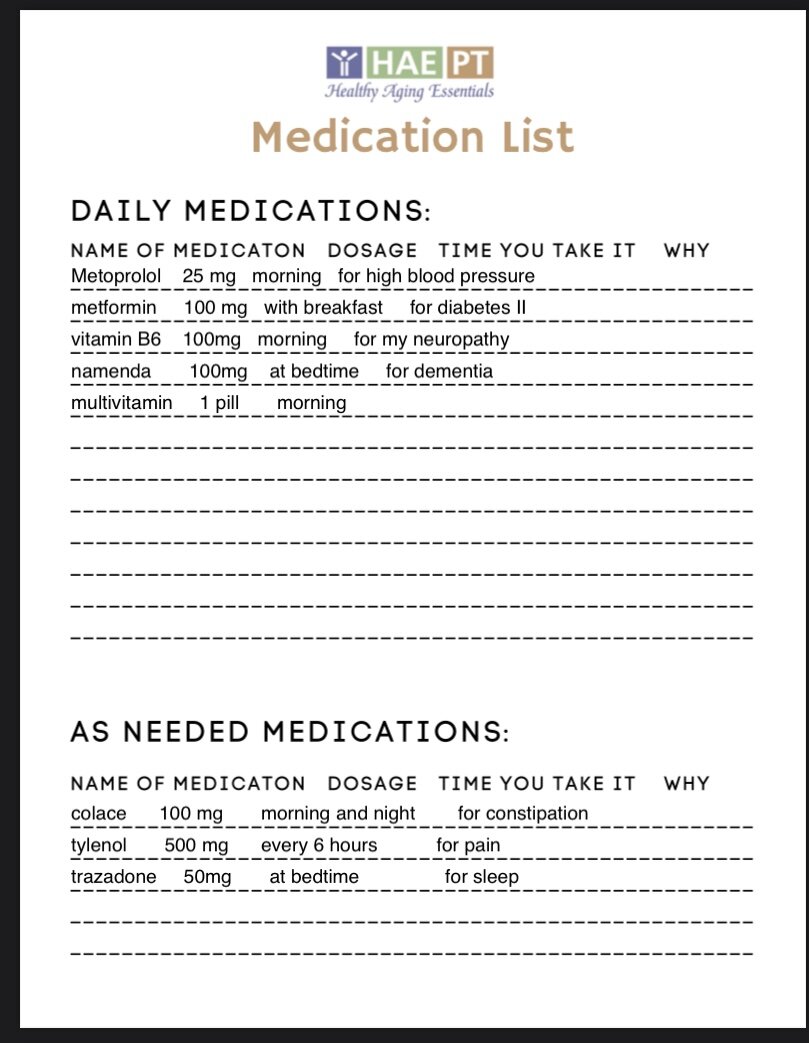
Your Medication List:
Daily Medications: Not just what you take, but how (by mouth, with food, on an empty stomach etc), how much (dosage and frequency), when you take it and most importantly, why. Is it to manage hypertension or your diabetes? What are the side effects you should be aware of? What should you do if you miss a dose? What if you take too many accidentally? It is helpful to know what the pill usually looks like, whether you take a generic or a brand and if you have a preference between the two.
As-needed or ‘PRN’ medications: What do you have on the list that you only take when you need it? For what reasons do you take this medication, and for how long? Do you need keep these on you, like a rescue inhaler or Nitro, or can you put them away somewhere for now to keep them out of the way?
Vitamins, supplements, inhalers, lotions, ointments and eye drops: These matter too! Make sure your physician knows any ‘extras’ you take because these, also, may interact with other medications on your list.
Allergies, Precautions and Dietary Considerations:
Allergies: Are you allergic to any foods or medications? What is your action plan if you experience an allergic reaction? Do you keep rescue medications on you at all times? Are they active and non-expired?
Precautions: Do you have any health conditions that require you to follow certain guidelines? Frequently, after a joint replacement or back surgery, your surgeon will ask you to follow certain rules to protect your healing tissues. Do you need to keep following these after you’ve healed or is it okay to resume your normal activities? Do you have any heart conditions that require you to keep your heart rate within certain ranges, or avoid drinking over a certain level of fluid each day?
Dietary Considerations: Are there any foods you need to avoid eating with your medications? Are there any dietary habits you should maintain to manage your chronic medical conditions? Believe it or not, even certain healthy foods can affect your medications if you are on a blood thinner (leafy greens and other foods high in Vitamin K are a no-no) and if you take medications like Levodopa to manage Parkinson’s, you’ll need to avoid taking them at the same time as protein or your body won’t digest the medication properly. Diabetics need to maintain a careful diet balancing sugar intake with insulin levels, and anyone with hypertension or congestive heart failure needs to be mindful of sodium intake. Dietary considerations vary from person to person - and you may have a number of conditions with contradicting guidelines, so having a conversation with a dietician may be a good place to start.
Current and Past Medical History:
Current Medical Problems: What conditions do you have that require ongoing medical management? Keep in mind, If you are taking a medication which adequately manages your medical condition, it doesn’t mean you no longer have it. For example. if you take a blood pressure medication, and no longer have high blood pressure because of it, it doesn’t mean you should take hypertension off of your current medical problem list. Any medical condition for which you either take a medication, monitor with a physician or manage through diet or exercise should remain on your current medical problem list. For each item on your list, you should be aware of which physician is responsible for management, which medications, if any, you take to manage it, and if there are any diet or exercise modifications you follow to keep it under control or from progressing. You should also be aware of any yellow or red flags that might indicate you may need medical attention. For example, if you have Congestive Heart Failure, you should know the name and number of your cardiologist, which medications you take to keep manage your fluid levels and blood pressure, how much water you are allowed to drink each day, and what signs or symptoms indicate you may be heading for an exacerbation like increased weight gain, shortness or breath or swelling in your ankles.
Past Medical History: This is the place for resolved or inactive medical problems you’ve experienced in the past. Things like an old knee replacement, appendicitis surgery or the time you had a UTI. Anything you place this list should not require ongoing management and should not cause any symptoms at this time.
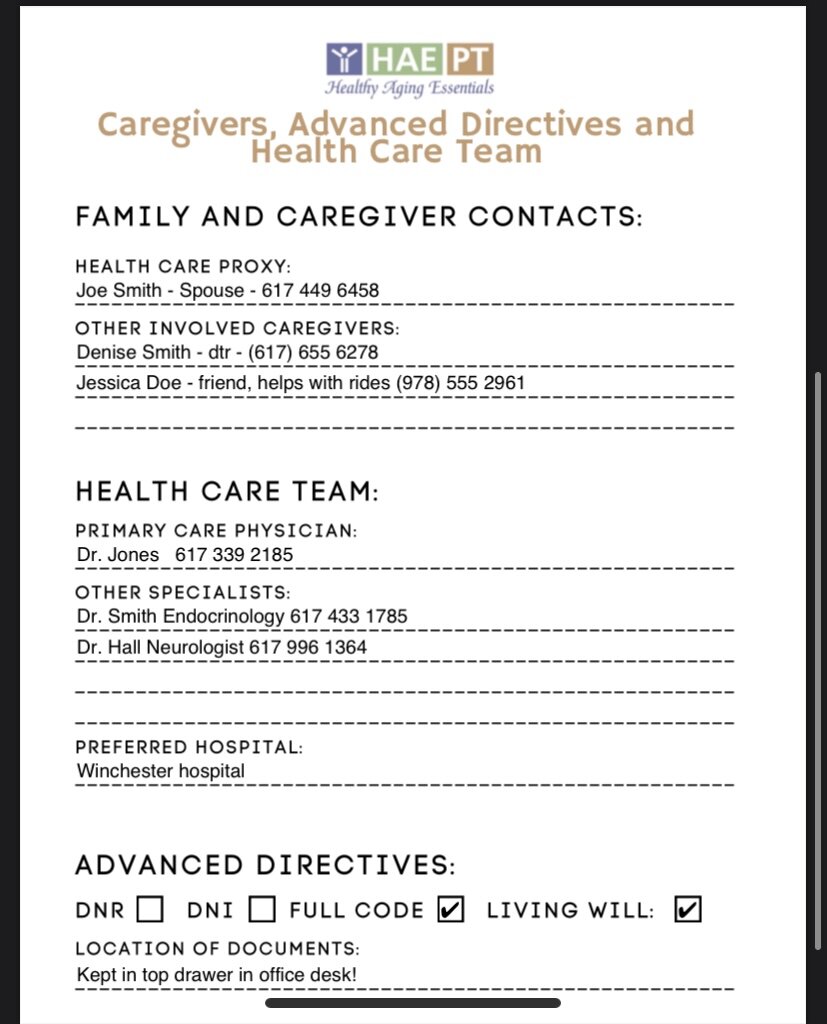
Family and Caregiver Contacts, Health Care Team and Advance Directives:
Family, Caregivers and Health Care Proxy: Who are your ‘people?’ If something goes wrong, or you rely on family or friends for help, who do you call? Who is your designated health care proxy? Keeping an active list, with current phone numbers for best contact, is a good habit and can help your healthcare team considerably if they need to reach out to someone who can help you.
Health Care Team: Who is your primary care physician and what specialists do you see to manage any chronic medical conditions? Do you have a preferred hospital or hospital network if you need to access emergent care? Is there a skilled nursing facility or acute rehab you’ve used in the past and had a good experience with? You may not always be given a choice, but generally paramedics will ask where you want to go, if they have the time to give you a choice.
Advanced Directives: What do you want someone to do if you have an emergency? Have you signed any advanced directives stating you do not want to be resuscitated in the event that your heart stops beating (DNR) or if you do not want to be intubated if you need assistance breathing (DNI)? Do you have a current Living Will in your home that further elaborates on your wishes if you are unable to provide them yourself? These forms are often signed during hospital stays and then forgotten about. Sometimes your wishes change. It is IMPERATIVE that you know what your wishes are, have them clearly stated in legal forms and have them accessible to the people who need to see them, when they need to see them. I recommend anyone who has an active DNR or DNI signed to post these on your refrigerator. This is the first place an EMT or other first responder will look if they come to your home and find you unresponsive. If it is not clear in your medical record or visible in line of sight, you will be resuscitated as if you were ‘full code’ and wanted to be saved. If you have a Living Will or other legal record, you should know where these are kept and have copies easily accessible for you or your loved one to find quickly if needed.
Signs of Poor Health Literacy
If you read through the above and felt like you had a handle on all of these issues, great! You’re well on your way to being adequately health-literate. It is a good idea to keep written records of all of the above, in an easy to spot location, as the last thing you or your loved one wants to do in an emergency is having to go searching through piles of paperwork. Still not sure how you rack up? Here are six other common signs of poor health literacy:
Frequent hospital admissions.
2. Poor management of chronic health conditions.
3. Forgetting medical appointments or missing regular follow up visits.
4. Trouble filling out health forms and past medical histories.
5. Frequent trouble with medications, like missing doses or running out of your pills too early.
6. Feelings of frustration with doctors, nurses and other healthcare workers.
If I now have you completely freaked out, fear not. There are easy ways to improve your health literacy and in turn, your overall health maintenance.
Tips to Improve Your Health Literacy
Ask questions and write down or record answers during your medical visits. Use your phone to take videos or auditory recordings so you can review them later if you need any clarification. Don’t be afraid to ask if you can repeat back what you think you heard so your healthcare team knows you've’ understood correctly.
Keep written health records on you or in easy-to-find locations. You should keep records of all the items above so you can easily provide them to EMTs, physicians or other members of your health care team if they need them. While most information is available online, keeping a hard copy will help you make sure you understand everything on ‘your list’ and remind you to ask about anything you don’t. Need an easy set of forms to keep it all organized? Check the HAE Store for a printable PDF of all the items above.
Use pill organizers or dispensers or utilize pharmacy pill packs. Pills get confusing! Make sure you have a system in place to make sure you take them at the right time - and a way to identify if you didn’t. Use phone timers and other reminders to cue you take pills when they’re scheduled.
Know what each medication you take is for and what common, or critical, side effects may be. If you have medication on your list, make sure you know why. What medical problem is it treating? Sometimes medications are prescribed for something years ago and may simply get ‘stuck’ there and may no longer be necessary. Ask questions of your physician, your pharmacist, or look them up online.
Be open and honest with your providers. Don’t be afraid to tell them how you feel, don’t be afraid of ‘being a pain,’ and if you feel like you can be open with your physician or other member of your healthcare team, it is time to find a new one. We can’t help you if we don’t know what’s going on.
Bring a trusted friend, family member or your health care proxy with you to your appointments. Whether they are there for emotional support, logistical support or to take notes for you, a second set of ears may not only be helpful, but necessary. If they can’t make it into the visit with you, ask if they can ‘Zoom’ or be there virtually.
Do you need some help organizing your medical information? You can download the forms I use to help my own patients organize their health information and medical histories at the HAE Patient and Therapist Store here:
Have an (Exercise) Snack..
If you’ve met me, been treated by me or ever visited my social media, you’re probably already aware that I strongly believe that Exercise is Medicine and that every adult should strive to meet the recommended 150-300 minutes a week of moderate intense exercise to prevent disease and better manage chronic conditions. However, only 1 of every 3 American Adults meet this recommendation, the rest, achieving less than that recommended dosage on a regular basis and placing themselves at increased risk for cardiovascular disease, diabetes and more.
A new study, published by Preventative Medicine Reports looks at a new approach to encouraging regular exercise in older adults. Given many older adults cite lack of time as a prohibiting factor, this study looked at prescribing exercise ‘snacks’ or small bouts of regular exercise every day. Participants in this study completed one minute of functional exercise (30 seconds of body-weight push ups and 30 seconds of squats), each and every day for 24 weeks. 75% of these of this group completed at least half of the sessions, and as a group, significant improvements were noted at the end of the trial in maximal push-up and squat performance.
You can read this study in it’s entirety here:
Take-home message? Even a little effort can yield positive results. Every day, I work with people limited by pain, disability and fear. Issuing an exercise program, and expecting compliance, to an older adult who hasn’t participated in regular exercise since they were young or who associates exercise with pain, fatigue or fall risk is one of the biggest challenges faced by Physical Therapists on a daily basis.
I frequently apply this idea of exercise ‘snacks’ to my patients, to help them gradually adjust to a more active lifestyle and too help them learn to see that exercise doesn’t have to be painful, exhausting or scary. I try to link these small bouts of exercise with everyday habits to make remembering to exercise second nature, and improve compliance. Whether you’re older and trying to get more active, or a therapist or other healthcare professional trying to help your client become healthier, you can try my top five favorite exercise snacks to get the ball rolling.
Sit to Stands - Every time you stand up off a chair, do it 5 times instead.
Counter Push Ups - Every time you walk by the kitchen sink, do 10 Counter Push Ups.
Single Leg Stand - Every time you brush your teeth, try to stand on one leg as long as you can.
Loaded Carries - After each meal, carry a soup cans in each hand and walk 5 laps back and forth across the kitchen.
Wall Angels - Put a post it note on a spot in the hallway and every time you pass it, perform 5 Wall Angels.
#haept #stronger #fitter #functional #physicaltherapist #physiotherapist #physicaltherapy #physiotherapy #doctorofphysicaltherapy #exercise #health #wellness #aging #healthyaging #optimalaging #successfulaging #exerciseismedicine #functionalstrength #balance #fallprevention #strengthtraining #freetalks #knowledgeispower #exercisesnacks
Happy 100th Birthday to the American Physical Therapy Association!
Happy 100 Years to the American Physical Therapy Association!
The APTA celebrates it’s 100th Birthday this year, though the roots of Physical Therapy go back way further. To honor this profession I’m so proud to be a part of, I wanted to share some interesting history on how it began and how it has continued to develop. The APTA has also developed some really cool resources on their APTA Centennial Page, like this timeline of 100 Milestones of Physical Therapy – APTA Centennial.
Old Old School History: In the BC times, even Hippocrates was hip to the benefits of manual therapy. In 460 BC, he documented the benefits of manual manipulation for pain relief and during the same era, in Ancient Greece, hydrotherapy became a thing when Hector began using water treatment to help people heal.
Old School History: Throughout the 1800’s, Sweden actually became the first country to establish an official PT registration through the National Health and Welfare Board and Physiotherapists used massage, manipulation and exercise to help gymnasts heal from injuries and illness.
Back in a century we actually lived in: The early 1900’s brought Physical Therapy to America. Rehabilitation aides and rehabilitation therapy was used to help soldiers recover after traumatic injuries sustained in World War 1, but the Polio epidemic in the 1920’s was where the benefits of Physical Therapy really took hold. Much like the current pandemic crisis we are living through, Polio shook our nation because in the absence of a vaccine, this paralytic virus had little mercy and killed thousands, and left many others paralyzed and often unable to breathe effectively without assistance - see the picture below of the Iron Lung! Physical Therapists helped people with polio learn to walk again with braces and crutches, and regain strength to get back to their normal lives. In 1921, Mary McMillan, the ‘Mother of Physical Therapy,’ established the American Women’s Physical Therapeutic Association, and the papers began to be published regarding the effects of physical therapy on healing and recovery.
Since then: The profession of Physical Therapy has continued to grow, specialize and diversify since then. Influential therapists have conducted careful research on the benefits of therapy and our profession has grown from women in dresses in black and white images helping children learn to walk to Doctors of Physical Therapy with advanced educations and certifications who hold Direct Access to see patients first because of our competence not only in healing, but in effectively triaging those who are appropriate and can benefit from conservative care from those who need further medical workup and treatment first. We are specialists in our respective fields: the APTA offers board-certified specialization in Cardiovascular and Pulmonary care, Geriatrics, Orthopedics, Neurology, Oncology, Pediatrics, Sports, Women’s Health and Wound Management. We work in hospitals, emergency rooms, private practices, on sports fields and in people’s homes. We help people of all ages recover strength and motor control, develop critical skills like mobility and walking after traumatic injuries, manage pain and teach self-management of chronic conditions and work with patients to live their fullest and best lives despite whatever physical limitations they may develop. I’m as proud as I’ve ever been to be part of this wonderful profession full of compassionate and caring individuals who truly live to make people feel better.
FAQ # 4: How Do I Know if I’m at ‘Fall Risk?’
As you know, I love to counter a question with another question, or in this case, three:
1 ) Have you fallen in the past year?
2) Do you feel unsteady with standing or walking?
3) Do you worry about falling?
If the answer to any of these is yes, research has shown that you are likely at an increased risk for falling. Now while this may seem like a short and sweet, the actual answer is a bit longer and more involved. This is where I come in. When I check to see if a patient of mine is at increased risk of falls, I’m like a detective on a trail. While I may start with these questions, their answers lead me down windy trails where I pick up clues that not only determine IF you are at fall risk, but more importantly, WHY. And it’s the WHY that allows me to help you prevent them. But that’s a story for a different post.
As you know, I love to counter a question with another question, or in this case, three:
1 ) Have you fallen in the past year?
2) Do you feel unsteady with standing or walking?
3) Do you worry about falling?
If the answer to any of these is yes, research has shown that you are likely at an increased risk for falling. Now while this may seem like a short and sweet, the actual answer is a bit longer and more involved. This is where I come in. When I check to see if a patient of mine is at increased risk of falls, I’m like a detective on a trail. While I may start with these questions, their answers lead me down windy trails where I pick up clues that not only determine IF you are at fall risk, but more importantly, WHY. And it’s the WHY that allows me to help you prevent them. But that’s a story for a different post.
So, back to the question at hand. What do I look at to determine if you’re at risk for falls?
1) I look at how you move. First and foremost, I look at your mobility, in your own home environment, sometimes when you don’t even think I’m watching (‘hey, can you give me a tour of your house?’). Without even doing another test, this would probably give me the most valuable information I can get. Do you stumble over thresholds? Reach for walls? Get distracted and lose balance with turning? Are there environmental hazards (small pets, throw rugs and more egads!) that could cause you trouble down the road? Is it dark? Is it too bright? Are you moving too fast, or too slow? Are you using assistive devices or may benefit from one? Do your movement patterns indicate an area of weakness or contracture? As therapists, this is our bread and butter. If you’re every hanging with a PT and feel like you’re being watched (or judged), you are! We can’t help ourselves, and we’re truly sorry:)
2) I look at your balance. Obvi. Your very ability to stand upright, balanced over your base of support requires an intricate and functioning relationship between your feet, your inner ear, your eyes and your brain. This combination is lovingly referred to as your somatosensory integration. It allows you to stay upright, and then allows you to control your body as it moves both purposely outside your base of support - and unpurposely (is that a word?), as in the case of a loss of balance. By putting you in a series of different foot positions, with different degrees of challenge to each of these systems (somatosensory, vestibular, visual), I can identify which system is working and which system could work better - and then develop a plan of action to improve your balance over all.
3) I look at aaaaallll other systems that are involved with your balance. Do you have pain that surprises you and knocks you off your feet? Limited range of motion in places that make your feet more likely to catch on the stair? Do you get tired easily or have impairments in cardiovascular function that make it more likely for you to pass out? Are you taking medicines that could make you dizzy, or confused or sleepy? Are you taking medicines that make it more likely to get injured from a fall like steroids that can make your bones more brittle or a blood thinner that could put you at risk for a head injury? Do you have other comorbidities that could play a role? Diabetes with fluctuating blood sugars? COPD with oxygen rates that drop when you move? Covid that has left you exhausted and uncertain on your feet?
Before this FAQ becomes a book, I’ll stop there. As you can tell, there is a lot that goes into answering this seemingly simple question. Fortunately, there are Physical Therapists, like me, who train for years to become Fall Risk Detection experts and are happy to help you figure it out. If you’d like to learn more about fall risk, fall prevention and how I figure this all out, please join me Tuesday night for a Zoom webinar titled ‘So You’ve Been Told You’re UNSTEADI. Now What?’ During this one-hour seminar, I’ll dive deeper into the fall risk assessment process, explain the STEADI initiative, and how it is used by your medical team to determine fall risk and address modifiable risk factors and give you tools to make changes on your own to help you stay on your feet.
To register ahead, please click the link below and you’ll receive the zoom link from there.
So You've Been Told You're UNSTEADI Zoom Registration