What is Health Literacy - and Why Does it Matter?
During a library talk last week, I spoke on the topic of Health Literacy. As life would have it, the day I was scheduled to present, I found myself dealing with a real-life example with a patient of why having a good grasp on health literacy is so critical to healthy aging. During our visit, I realized my patient had been taking double the dose of her prescribed medication - not out of any error on her part, but because she had two prescriptions on file for the same medication, one for the generic version, and one for the brand name - and she was unaware they were the same drug. How does this happen? How did this get by so many layers of well-meaning and conscientious health care professionals and hospital settings? Unfortunately, this stuff happens, and happens all too often, because there are a lot of ‘cooks in the kitchen’ and because all of us ‘cooks’ are human and we make mistakes. But this, this is why it is so imperative for you as the consumer, as the patient, to have an adequate level of health literacy - so you can be your own advocate, so you can be on the lookout for medical errors and so you can play an active, instead of passive, role in your own health maintenance.
What is Health Literacy?
“Health literacy is the ability to obtain, read, understand and use healthcare information in order to make appropriate health decisions and follow instructions for treatment.” (Wikipedia).
Sounds simple enough, right? It may be simple enough if you have one or maybe two medical diagnoses, or take a pill or two in the morning. But what happens when the list starts to add up? When you’re taking pills in the morning, a few after lunch and one before bed? When the instructions come from more than just your primary care physician, but also from your cardiologist or neurologist? If you’ve ever been discharged from the hospital, you’ve had the experience of being issued a stack of papers to sign with discharge recommendations, red flags to be aware of, with a current medication list (which may have new pills or have old pills crossed off) and visits you’ll need to attend in the future. This experience alone is overwhelming. Add in confusion, fatigue, pain or anxiety related to your hospital stay and you now have a recipe for disaster. It is REALLY HARD to keep track of it all, and even harder to keep up with the changes that are often part of getting older and dealing with chronic diseases, new diagnoses, illnesses and injuries.
How do you know if you are adequately health literate?
You may be responsible for not only your health information management, but also for a spouse or aging parent.
At the minimum, to be health-literate, you should have a solid grasp on the following:
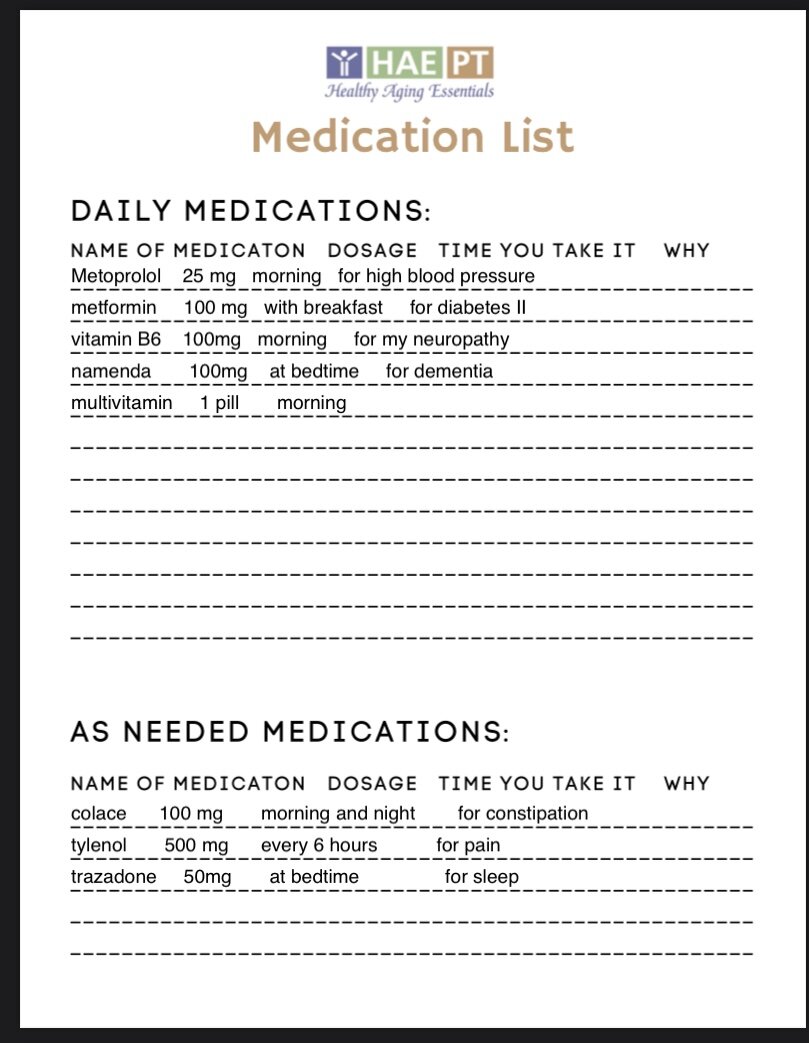
Your Medication List:
Daily Medications: Not just what you take, but how (by mouth, with food, on an empty stomach etc), how much (dosage and frequency), when you take it and most importantly, why. Is it to manage hypertension or your diabetes? What are the side effects you should be aware of? What should you do if you miss a dose? What if you take too many accidentally? It is helpful to know what the pill usually looks like, whether you take a generic or a brand and if you have a preference between the two.
As-needed or ‘PRN’ medications: What do you have on the list that you only take when you need it? For what reasons do you take this medication, and for how long? Do you need keep these on you, like a rescue inhaler or Nitro, or can you put them away somewhere for now to keep them out of the way?
Vitamins, supplements, inhalers, lotions, ointments and eye drops: These matter too! Make sure your physician knows any ‘extras’ you take because these, also, may interact with other medications on your list.
Allergies, Precautions and Dietary Considerations:
Allergies: Are you allergic to any foods or medications? What is your action plan if you experience an allergic reaction? Do you keep rescue medications on you at all times? Are they active and non-expired?
Precautions: Do you have any health conditions that require you to follow certain guidelines? Frequently, after a joint replacement or back surgery, your surgeon will ask you to follow certain rules to protect your healing tissues. Do you need to keep following these after you’ve healed or is it okay to resume your normal activities? Do you have any heart conditions that require you to keep your heart rate within certain ranges, or avoid drinking over a certain level of fluid each day?
Dietary Considerations: Are there any foods you need to avoid eating with your medications? Are there any dietary habits you should maintain to manage your chronic medical conditions? Believe it or not, even certain healthy foods can affect your medications if you are on a blood thinner (leafy greens and other foods high in Vitamin K are a no-no) and if you take medications like Levodopa to manage Parkinson’s, you’ll need to avoid taking them at the same time as protein or your body won’t digest the medication properly. Diabetics need to maintain a careful diet balancing sugar intake with insulin levels, and anyone with hypertension or congestive heart failure needs to be mindful of sodium intake. Dietary considerations vary from person to person - and you may have a number of conditions with contradicting guidelines, so having a conversation with a dietician may be a good place to start.
Current and Past Medical History:
Current Medical Problems: What conditions do you have that require ongoing medical management? Keep in mind, If you are taking a medication which adequately manages your medical condition, it doesn’t mean you no longer have it. For example. if you take a blood pressure medication, and no longer have high blood pressure because of it, it doesn’t mean you should take hypertension off of your current medical problem list. Any medical condition for which you either take a medication, monitor with a physician or manage through diet or exercise should remain on your current medical problem list. For each item on your list, you should be aware of which physician is responsible for management, which medications, if any, you take to manage it, and if there are any diet or exercise modifications you follow to keep it under control or from progressing. You should also be aware of any yellow or red flags that might indicate you may need medical attention. For example, if you have Congestive Heart Failure, you should know the name and number of your cardiologist, which medications you take to keep manage your fluid levels and blood pressure, how much water you are allowed to drink each day, and what signs or symptoms indicate you may be heading for an exacerbation like increased weight gain, shortness or breath or swelling in your ankles.
Past Medical History: This is the place for resolved or inactive medical problems you’ve experienced in the past. Things like an old knee replacement, appendicitis surgery or the time you had a UTI. Anything you place this list should not require ongoing management and should not cause any symptoms at this time.
Family and Caregiver Contacts, Health Care Team and Advance Directives:
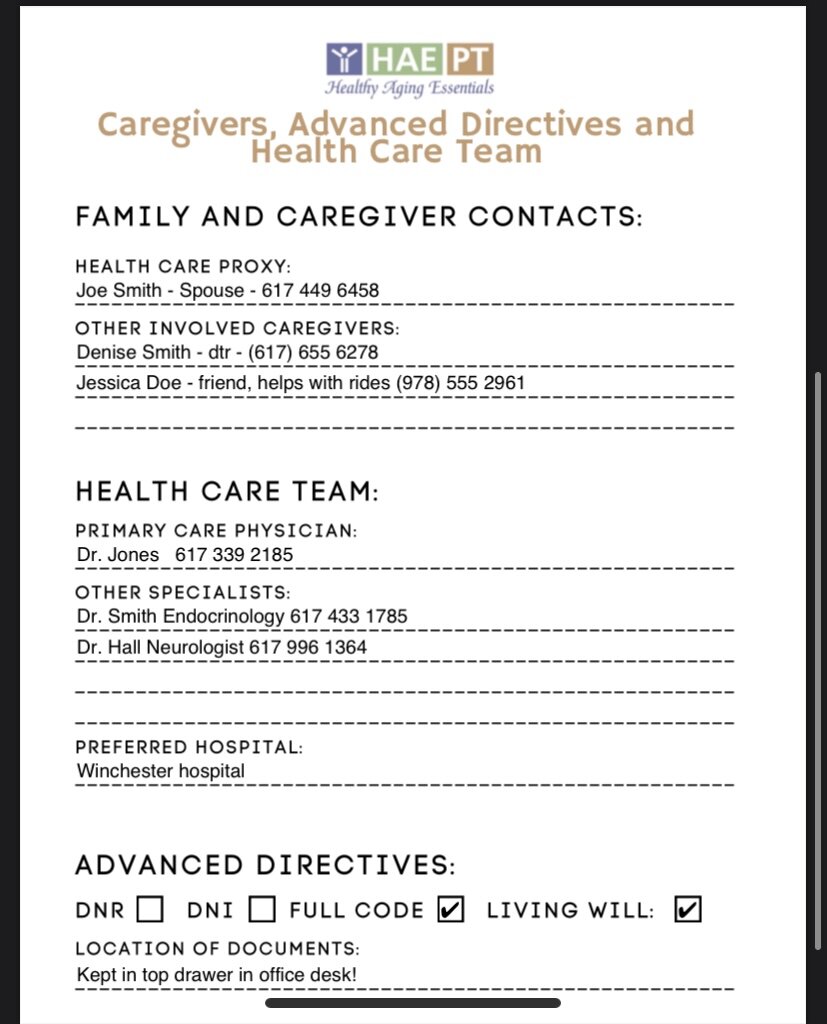
Family, Caregivers and Health Care Proxy: Who are your ‘people?’ If something goes wrong, or you rely on family or friends for help, who do you call? Who is your designated health care proxy? Keeping an active list, with current phone numbers for best contact, is a good habit and can help your healthcare team considerably if they need to reach out to someone who can help you.
Health Care Team: Who is your primary care physician and what specialists do you see to manage any chronic medical conditions? Do you have a preferred hospital or hospital network if you need to access emergent care? Is there a skilled nursing facility or acute rehab you’ve used in the past and had a good experience with? You may not always be given a choice, but generally paramedics will ask where you want to go, if they have the time to give you a choice.
Advanced Directives: What do you want someone to do if you have an emergency? Have you signed any advanced directives stating you do not want to be resuscitated in the event that your heart stops beating (DNR) or if you do not want to be intubated if you need assistance breathing (DNI)? Do you have a current Living Will in your home that further elaborates on your wishes if you are unable to provide them yourself? These forms are often signed during hospital stays and then forgotten about. Sometimes your wishes change. It is IMPERATIVE that you know what your wishes are, have them clearly stated in legal forms and have them accessible to the people who need to see them, when they need to see them. I recommend anyone who has an active DNR or DNI signed to post these on your refrigerator. This is the first place an EMT or other first responder will look if they come to your home and find you unresponsive. If it is not clear in your medical record or visible in line of sight, you will be resuscitated as if you were ‘full code’ and wanted to be saved. If you have a Living Will or other legal record, you should know where these are kept and have copies easily accessible for you or your loved one to find quickly if needed.
Signs of Poor Health Literacy
If you read through the above and felt like you had a handle on all of these issues, great! You’re well on your way to being adequately health-literate. It is a good idea to keep written records of all of the above, in an easy to spot location, as the last thing you or your loved one wants to do in an emergency is having to go searching through piles of paperwork. Still not sure how you rack up? Here are six other common signs of poor health literacy:
Frequent hospital admissions.
2. Poor management of chronic health conditions.
3. Forgetting medical appointments or missing regular follow up visits.
4. Trouble filling out health forms and past medical histories.
5. Frequent trouble with medications, like missing doses or running out of your pills too early.
6. Feelings of frustration with doctors, nurses and other healthcare workers.
If I now have you completely freaked out, fear not. There are easy ways to improve your health literacy and in turn, your overall health maintenance.
Tips to Improve Your Health Literacy
Ask questions and write down or record answers during your medical visits. Use your phone to take videos or auditory recordings so you can review them later if you need any clarification. Don’t be afraid to ask if you can repeat back what you think you heard so your healthcare team knows you've’ understood correctly.
Keep written health records on you or in easy-to-find locations. You should keep records of all the items above so you can easily provide them to EMTs, physicians or other members of your health care team if they need them. While most information is available online, keeping a hard copy will help you make sure you understand everything on ‘your list’ and remind you to ask about anything you don’t. Need an easy set of forms to keep it all organized? Check the HAE Store for a printable PDF of all the items above.
Use pill organizers or dispensers or utilize pharmacy pill packs. Pills get confusing! Make sure you have a system in place to make sure you take them at the right time - and a way to identify if you didn’t. Use phone timers and other reminders to cue you take pills when they’re scheduled.
Know what each medication you take is for and what common, or critical, side effects may be. If you have medication on your list, make sure you know why. What medical problem is it treating? Sometimes medications are prescribed for something years ago and may simply get ‘stuck’ there and may no longer be necessary. Ask questions of your physician, your pharmacist, or look them up online.
Be open and honest with your providers. Don’t be afraid to tell them how you feel, don’t be afraid of ‘being a pain,’ and if you feel like you can be open with your physician or other member of your healthcare team, it is time to find a new one. We can’t help you if we don’t know what’s going on.
Bring a trusted friend, family member or your health care proxy with you to your appointments. Whether they are there for emotional support, logistical support or to take notes for you, a second set of ears may not only be helpful, but necessary. If they can’t make it into the visit with you, ask if they can ‘Zoom’ or be there virtually.